A Comprehensive Review of Spondylolisthesis: Pathophysiology, Classification, and Management
Abstract Spondylolisthesis is a spinal condition characterised by the forward displacement of one vertebra over another. This article provides a comprehensive review of the pathophysiology, anatomical considerations, classification based on the degree of slippage, treatment modalities, and surgical management. Emphasis is placed on the use of instrumentation in surgical interventions, with an overview of current advancements.
1. Introduction Spondylolisthesis is a common spinal disorder with varying aetiologies, including congenital defects, degenerative changes, trauma, and spondylolysis. This condition may lead to instability, pain, neurological deficits, and functional impairment, necessitating a well-structured diagnostic and therapeutic approach (Wiltse et al., 1976).
2. Anatomy and Pathophysiology The spine consists of 33 vertebrae, of which the lumbar region is most susceptible to spondylolisthesis due to its load-bearing function and mobility. The pathophysiology of spondylolisthesis involves the failure of the pars interarticularis (as in isthmic spondylolisthesis) or progressive facet joint degeneration (as in degenerative spondylolisthesis) (Matsunaga et al., 2000). The mechanical instability leads to altered biomechanics, resulting in increased stress and further displacement.
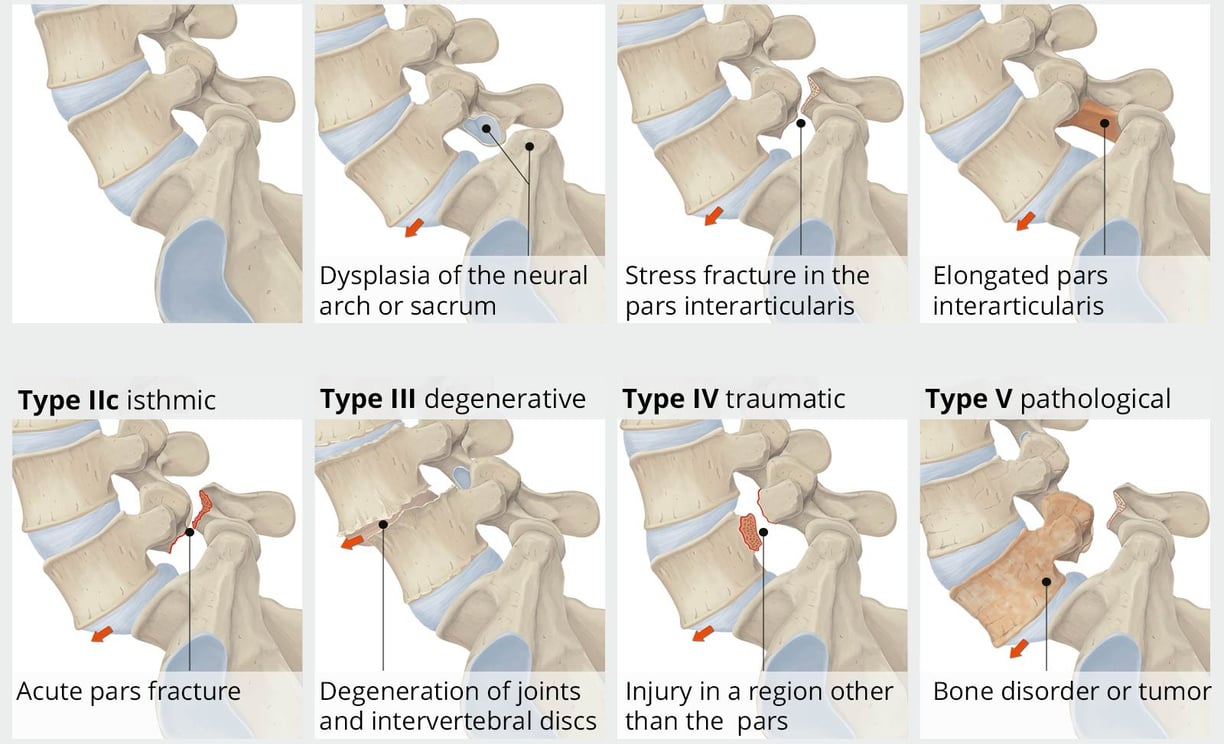
3. Classification and Degree of Slippage Spondylolisthesis is classified based on the Wiltse-Newman system into:
Dysplastic (congenital)
Isthmic (due to pars defect)
Degenerative (facet and disc degeneration)
Traumatic (acute fracture)
Pathologic (due to disease or tumour)
Iatrogenic (post-surgical instability) (Wiltse et al., 1976).
The degree of slippage is graded using the Meyerding classification:
Grade I: < 25% slippage
Grade II: 25-50% slippage
Grade III: 50-75% slippage
Grade IV: 75-100% slippage
Grade V (Spondyloptosis): Complete slippage (Meyerding, 1932).
4. Clinical Presentation and Diagnosis Patients may present with lower back pain, radiculopathy, neurogenic claudication, or cauda equina syndrome in severe cases. Diagnosis is confirmed through imaging studies such as X-rays (dynamic views), MRI (soft tissue involvement), and CT scans (bony detail) (Mac-Thiong et al., 2018).
5. Conservative Management Non-surgical treatment is indicated for low-grade spondylolisthesis and includes:
Activity modification
Physiotherapy (core strengthening and postural training)
Analgesics and anti-inflammatory medications
Epidural steroid injections for symptomatic relief (Matsunaga et al., 2000).
6. Surgical Management and Instrumentation Surgery is indicated in cases of progressive slippage, neurological deficits, or failed conservative treatment. Surgical options include:
Decompression Alone: Reserved for cases without significant instability.
Decompression with Fusion: Gold standard for stabilisation, commonly using posterior lumbar interbody fusion (PLIF) or transforaminal lumbar interbody fusion (TLIF) (Glassman et al., 2012).
Instrumentation:
Pedicle screw fixation: Enhances spinal stability and fusion rates.
Interbody cages: Used to restore disc height and alignment.
Minimally invasive techniques: Reducing surgical morbidity (Bridwell & DeWald, 2011).
7. Postoperative Care and Outcomes Patients require structured rehabilitation post-surgery, including early mobilisation and physiotherapy. Outcomes depend on the severity of slippage, surgical technique, and adherence to postoperative guidelines (Glassman et al., 2012).
8. Conclusion Spondylolisthesis is a multifaceted condition requiring a tailored approach to management. Advances in surgical techniques and instrumentation have improved patient outcomes, particularly in high-grade cases.
References
Bridwell, K. H., & DeWald, R. L. (2011). The textbook of spinal surgery (3rd ed.). Lippincott Williams & Wilkins.
Glassman, S. D., Carreon, L. Y., & Campbell, M. J. (2012). The impact of instrumented fusion on spondylolisthesis treatment outcomes. Spine Journal, 12(2), 121-130.
Kalichman, L., Hunter, D. J., & Dennerlein, J. T. (2009). Spondylolysis and spondylolisthesis: Prevalence and risk factors in a community-based study. Spine, 34(2), 199-205.
Mac-Thiong, J. M., Wang, Z., & Parent, S. (2018). Spondylolisthesis: Classification, pathophysiology, and natural history. Neurosurgery Clinics of North America, 29(3), 303-310.
Matsunaga, S., Ijiri, K., & Hayashi, K. (2000). Nonsurgical treatment of lumbar spondylolisthesis: Clinical and radiological analysis of 45 cases. Spine, 25(13), 1710-1715.
Meyerding, H. W. (1932). Spondylolisthesis: Surgical treatment and results. Journal of Bone and Joint Surgery, 14(4), 841-850.
Rosenberg, N. J. (1975). Degenerative spondylolisthesis: Predisposing factors. Journal of Bone and Joint Surgery, 57(4), 467-474.
Wiltse, L. L., Newman, P. H., & Macnab, I. (1976). Classification of spondylolysis and spondylolisthesis. Clinical Orthopaedics and Related Research, 117, 23-29.
Contact
Schedule your consultation with our expert team.
Resources
info@thebrainandspine.com
123-456-7890
© 2024. All rights reserved.