Cervical Radiculopathy: Causes, Diagnosis, and Treatment.
Introduction
Cervical radiculopathy, commonly referred to as radicular nerve pain, results from irritation or compression of spinal nerve roots in the cervical spine. This condition can cause pain, numbness, and weakness radiating along the affected nerve distribution. It is a frequent cause of neck, shoulder, and arm pain and can significantly impact a patient’s quality of life.
Commonly Affected Levels and Pain Distribution
Cervical radiculopathy most frequently affects the following nerve roots:
C5 Nerve Root (C4-C5 Disc Herniation): Pain radiates from the neck to the lateral shoulder and upper arm. Patients may experience deltoid weakness and diminished biceps reflex.
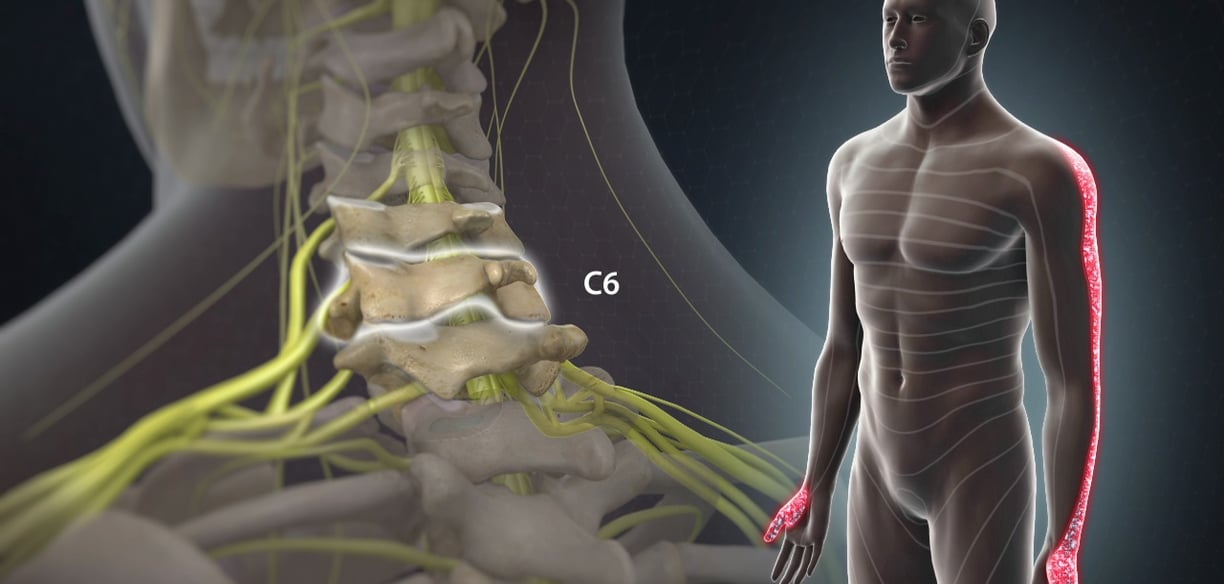
C6 Nerve Root (C5-C6 Disc Herniation): Pain extends from the neck to the lateral forearm and thumb. Weakness in wrist extension and biceps may be noted, with a reduced brachioradialis reflex.
C7 Nerve Root (C6-C7 Disc Herniation): Pain follows the posterior arm, dorsum of the forearm, and extends into the middle finger. Weakness in triceps and wrist flexion, along with a diminished triceps reflex, is common.
C8 Nerve Root (C7-T1 Disc Herniation): Pain affects the medial forearm, ring, and little fingers. Weakness in finger flexors and intrinsic hand muscles may be noted.
Differential Diagnoses
Several conditions can mimic cervical radiculopathy and should be considered:
Brachial Plexopathy: Often presents with broader nerve involvement beyond a single root distribution.
Thoracic Outlet Syndrome: Can cause similar upper extremity pain and weakness due to vascular or neurogenic compression.
Peripheral Neuropathy: Diffuse rather than dermatomal distribution of symptoms.
Rotator Cuff Pathology: Shoulder pain without neurological deficits, often confused with C5 radiculopathy.
Multiple Sclerosis: May present with sensory changes and weakness mimicking radiculopathy.
Treatment Options
Management of cervical radiculopathy follows a stepwise approach, ranging from conservative care to surgical intervention when necessary.
1. Conservative Treatment
Activity Modification: Avoiding activities that exacerbate symptoms while maintaining mobility.
Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation.
Neuropathic agents (gabapentinoids, tricyclic antidepressants) for nerve pain modulation.
Short courses of oral corticosteroids in acute exacerbations.
Physical Therapy:
Strengthening exercises for neck and shoulder muscles.
Cervical traction to reduce nerve root compression.
Postural correction and ergonomic education.
2. Minimally Invasive Interventions
Epidural Steroid Injections (ESIs):
Corticosteroid injections near the affected nerve root to reduce inflammation and provide temporary pain relief.
Particularly beneficial for acute radicular pain unresponsive to conservative measures.
Selective Nerve Root Blocks:
Targeted injection of local anaesthetic and corticosteroids around a specific nerve root for diagnostic and therapeutic purposes.
3. Surgical Intervention
Surgery is considered when conservative and minimally invasive treatments fail, particularly in cases of significant neurological deficits or severe, persistent pain.
Indications for Surgery:
Progressive or severe motor weakness (e.g., loss of grip strength due to C8 nerve root compression).
Intractable pain despite 6-12 weeks of conservative treatment.
Myelopathy due to spinal cord compression, presenting with:
Gait disturbances.
Bowel and/or bladder dysfunction.
Upper motor neuron signs (hyperreflexia, spasticity).
Surgical Options:
Anterior Cervical Discectomy and Fusion (ACDF):
Removal of herniated disc material and fusion of adjacent vertebrae.
Preferred for single or multilevel disc pathology causing severe radicular pain.
Cervical Disc Replacement:
Preserves motion at the affected level while decompressing the nerve root.
Posterior Foraminotomy:
Removal of bone spurs or disc material compressing the nerve root without fusion.
Conclusion
Cervical radiculopathy is a common yet potentially debilitating condition resulting from nerve root compression in the cervical spine. A thorough understanding of pain distribution, differential diagnoses, and treatment modalities is essential for optimal management. Conservative treatments are effective in most cases, but minimally invasive procedures and surgical intervention may be required for persistent or severe symptoms.
References
Deyo RA, et al. (2014). "Managing Neck Pain and Cervical Radiculopathy: Evidence-Based Approaches." New England Journal of Medicine, 371(16), 1552-1563.
Ropper AH, et al. (2015). "Cervical Radiculopathy and Spinal Disorders." New England Journal of Medicine, 372(14), 1240-1248.
Kreiner DS, et al. (2020). "Guidelines for the Management of Cervical Disc Herniation with Radiculopathy." Spine Journal, 20(1), 135-148.
Matz PG, et al. (2009). "Surgical Versus Non-Surgical Treatment for Cervical Radiculopathy: A Meta-Analysis." Spine (Phila Pa 1976), 34(4), 816-823.

Contact
Schedule your consultation with our expert team.
Resources
info@thebrainandspine.com
123-456-7890
© 2024. All rights reserved.